Learn how the ET3 Model will transform emergency medicine — and how it works hand in hand with UCM’s Virtual ER

The Center for Medicare and Medicaid Innovation recently introduced a voluntary, five-year payment model called Emergency Triage, Treat, and Transport (ET3), in order to provide greater flexibility to ambulance care teams to address emergency health care needs of Medicare beneficiaries following a 911 call. Under the ET3 model, the Centers for Medicare & Medicaid Services (CMS) will pay participating ambulance suppliers and providers to:
- transport an individual to a hospital emergency department (ED) or other destination covered under the regulations
- transport to an alternative destination (such as a primary care doctor’s office or an urgent care clinic)
- provide treatment in place with a qualified health care practitioner, either on the scene or connected using telehealth
The model will allow beneficiaries to access the most appropriate emergency services at the right time and place. This model complements the heart of the UCM model: our Virtual ER provides triage, treatment and data analytics and can help any organization looking to participate in ET3.
Some background:
For more than 50 years, Emergency Medicine has operated with in the four walls of a hospital and this newly announced model of care will help bring the emergency room to patients wherever they are; The Center for Medicare and Medicaid Innovation (CMMI) — the innovation arm of the Centers for Medicare and Medicaid Services (CMS) — put the world on notice on February 14 that it’s time for a change. Emergency Triage, Treat, and Transport (ET3) is a five-year demonstration project that will allow ambulance teams to get paid for triage and treatment of fee-for-service Medicare beneficiaries in the home and for taking them to a doctor’s office or an urgent care center, rather than to an emergency department (ED).
Today, as another example of how incentives in our healthcare system are backwards, most insurers, including Medicare, pay for ambulance services only when patients who call 911 are taken to hospitals. They’re transported to the ED, even when no care or a lower-acuity-care setting may be more appropriate.
Under the new model, when emergency medical services (EMS) providers arrive at a patient’s residence after a 911 call, they may triage the patient to care at home, an ED, a doctor’s office, an urgent care center, or a hospital emergency room. If the patient wants to go to the hospital, the EMS team must honor that person’s wishes. When medically appropriate, the patient may be treated right there on the spot by an EMS professional through a telehealth consultation.
Starting in 2020, the demonstration will study whether the new ET3 model can safely reduce unnecessary use of EDs by fee-for-service Medicare patients. CMMI is encouraging participants in the program to partner with other payers, including state Medicaid programs, to provide similar interventions to patients in their geographic areas.
Let’s take a look at how it works:
911 dispatch services, whether operated by a local government or some other entity, will have the opportunity to create government-funded medical triage lines in areas where the model is being tested. When a Medicare beneficiary calls 911 and is connected to a dispatch system that has incorporated a medical triage line, the individual will be screened for eligibility for triage services simultaneously with the ambulance supplier being contacted.
Timing:
This summer, Medicare-enrolled ambulance suppliers and providers in certain regions will be asked to apply for participation in the ET3 model. By the fall decisions will begin to be made.
CMMI will phase in the ET3 model in an unspecified number of regions. The agency will conduct up to three rounds of requests for ambulance applications and up to two notices of funding opportunities for dispatch services with staggered start dates. Because the demonstration is limited to five years, only the ambulance and dispatch services that enroll during the initial rounds will be able to participate for the full period.
Benefits and goals:
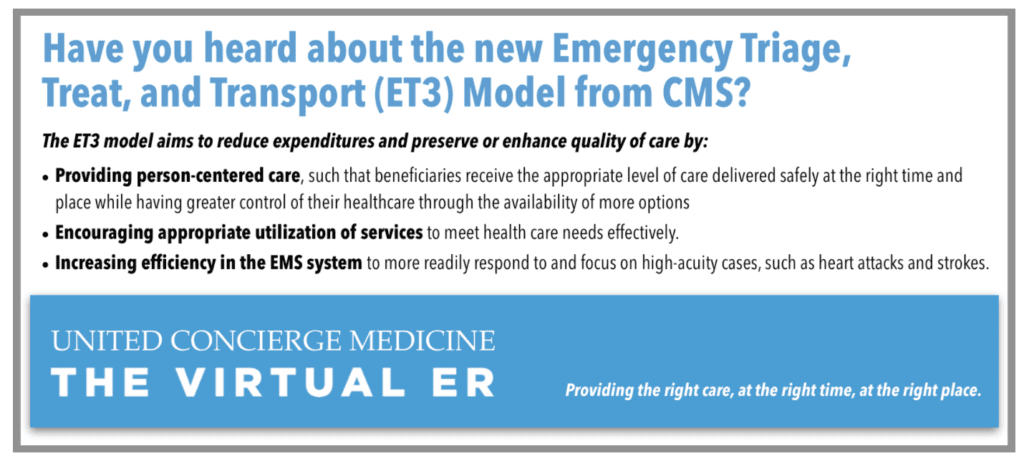
The goals of the ET3 demonstration, CMMI says, are to ensure the provision of person-centered care based on each patient’s needs, guarantee appropriate utilization of services, and increase the efficiency of the EMS system so that ambulances and EMS professionals can “more readily respond to and focus on high-acuity cases, such as heart attacks and strokes.”
Patients will be able to receive the right care, in the right place, at the right time and have lower copays when they are triaged to a care setting other than the ED, the agency notes. In addition, the model allows patients to avoid long wait times in the ED and exposure to hospital-acquired conditions. “This model will create a new set of incentives for emergency transport and care, ensuring patients get convenient, appropriate treatment in whatever setting makes sense for them,” said HHS Secretary Alex Azar in the news release.
We believe the although the concept of emergency medicine triage has been around hundreds of years, it is rarely implemented correctly. This historic moment in US healthcare is a critical step in fixing our broken healthcare system.
HOW UCM CAN HELP:
UCM provides thousands of in-home virtual emergency departments visits each month through out Virtual ER. ET3 participants can gain use of our technology and ER service, including our 24/7/365 call center run by an experienced Emergency Medicine Team of ER physicians, Physician Assistants, Nurse Practitioners, nurses and EMTs who can diagnose, prescribe medication, and make critical triage decisions with our EMS partners. We then provide detailed data and analytics to demonstrate the healthcare improvement in quality and cost reduction necessary to turn any pilot program into a long-term sustainable model of emergency medicine triage.






